Abstract
Introduction: There is no consensus for when hereditary thrombophilia testing is indicated. When venous or arterial thrombotic events occur it is crucial to evaluate for provoking risk factors. Likely, genetic predisposition requires a double-hit event for thrombosis to occur. In the acute setting, Protein C and S, and Antithrombin III testing may not reliable. Whereas testing for Factor V Leiden or Prothrombin 20210A gene mutations may be reliable, however, the result is unlikely to change management of acute thrombosis. As such, there is potential for high cost with low yield, and false positives in inpatient thrombophilia testing.
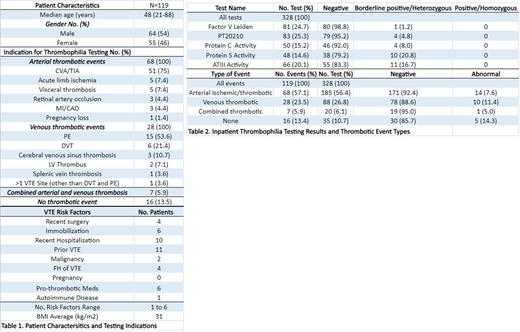
Methods: This was a retrospective, observational, study reviewing the indications, results, and patient characteristics of cases in which hereditary thrombophilia testing occurred. Indications for testing and influence of results on management were determined based on clinical documentation. These tests included FVL, PT20210A, Protein C and S, and ATIII. The study population included patients who were admitted to Augusta University Medical Center, an academic institution in Augusta, GA, in 2021. All patients were >18 years of age. ATIII testing for indications other than thrombophilia were excluded.
Results: 119 patients were identified, for whom 328 tests were ordered. The median age of patients was 48 years (21-88yo) with 54% being male. The most common indications for testing, 68 (57%), were arterial thrombotic events, with a total of 51 (75%) patients having a CVA or TIA. 25 of the 51 patients with CVA or TIA had at least one potential risk factor, most commonly being prior vascular events, TIIDM, and HTN. Other risk factors included acute illness from bacterial endocarditis and Covid-19 infection.
28 (24%) patients had an acute VTE event, with the most common indication being acute pulmonary embolism. All but one patient had at least one, to six, potential provoking factors or comorbidities that can be associated with VTE. This patient had CTA neck performed for evaluation of possible CVA or TIA. Incidentally, a possible internal jugular vein DVT was noted, however, a follow up doppler ultrasound exam failed to show a DVT. The most common risk factors included recent hospitalization and history of VTE. The average BMI for patients with VTE was 31kg/m2.
A total of 16 patients had at least one of these tests ordered in the absence of an apparent thrombotic event. With one exception there was clinical concern for thrombosis, including arterial or venous, however, an event was ultimately excluded. This patient was screened for FVL due to family history of thrombosis. Cases in which no thrombotic event had occurred included CVA having been ruled out, central line clotting, and renal transplant failure.
Of the 328 tests ordered, none were clearly positive or homozygous for a gene mutation. There were 30 tests that were borderline positive or heterozygous. 34 (29%) patients received therapeutic anticoagulation at the time of testing. With one exception, none of these impacted the decision to prescribe anticoagulation at discharge. This testing resulted in $113,483 in patient charges in 2021.
Conclusion: Arterial thrombotic events were the most common indication given, with many having a documented risk factor, and the results did not affect management. This reinforces the controversial role of thrombophilia testing, particularly in CVA and TIA. Thrombophilia evaluation is not recommended in provoked VTE and all, but one patient had a provoking risk factor. These data suggest a limited role and high cost for inpatient thrombophilia testing. They will be used to implement a tool to reduce this testing at Augusta University.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal